In 2014, NHS England’s ‘Five Year Forward View’ was published, a strategic plan that outlines the future direction and transformation of the NHS in England over the next five years.
The plan addressed the healthcare crisis by proposing new models of care. Among the proposals was embedding private sector expertise, such as UnitedHealth’s UK subsidiary Optum, into NHS operations and encouraging the digital transformation.
Among the digital and technological innovations was the development of “Healthy New Towns” with smart homes and integrated community health services. And not ashamed of using psychology on the public to bring about behavioural change, the plan also included the use of behavioural “nudges” and incentives, including programmes like BetterPoints, which reward “sustainable” travel choices.
“Sustainable” means the United Nations’ (“UN’s”) global agenda. BetterPoints programmes are designed to align with the UN’s Sustainable Development Goals and to help achieve them.
The NHS is deliberately being used as a tool to further the Globalists’ agenda.
Let’s not lose touch…Your Government and Big Tech are actively trying to censor the information reported by The Exposé to serve their own needs. Subscribe to our emails now to make sure you receive the latest uncensored news in your inbox…
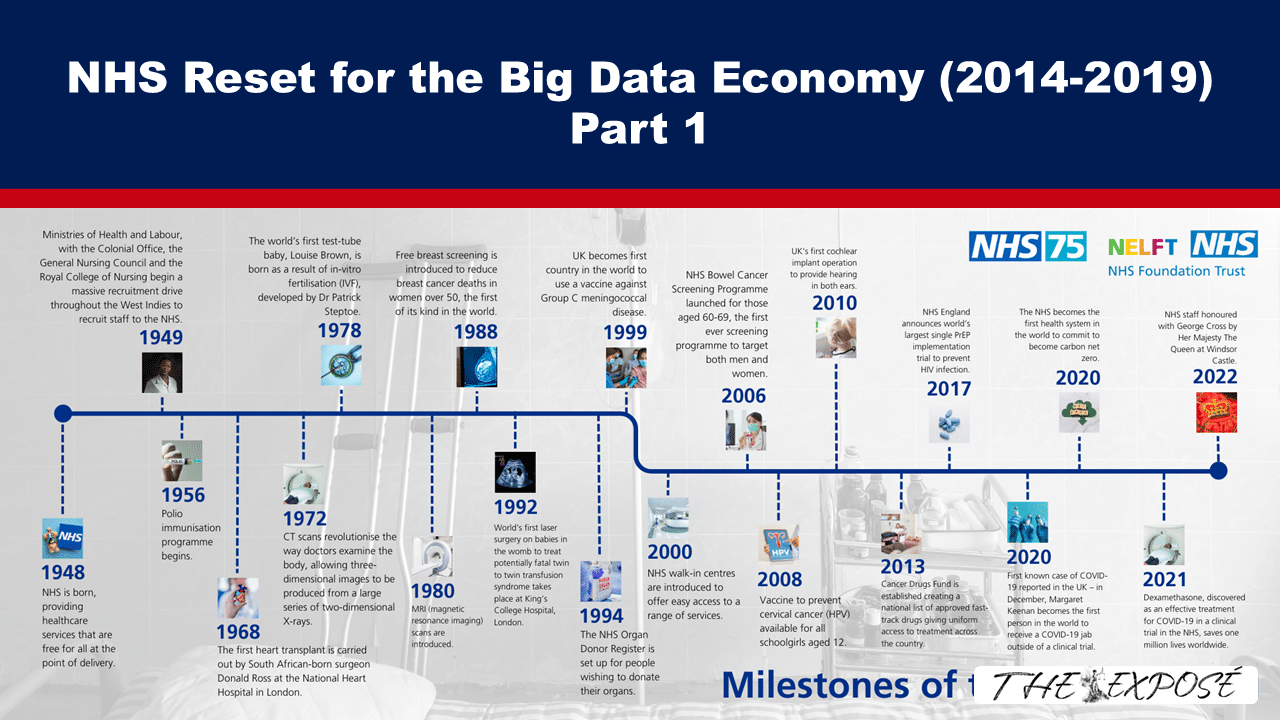
The Real Left is publishing a series of essays titled ‘The Health and Social Care Reset for the Big Data Economy’. You can read the first part, ‘The Great Health and Social Care Reset for the Big Data Economy Part 1.1’, which is a timeline of NHS capture during the years 1970s-2013, HERE.
The following is a section of the second part, which is a timeline of NHS capture during the years 2014-2019. We have published the essay in several parts because, totalling a little under 10,500 words, it’s longer than most would read in a single sitting.
The Great Health and Social Care Reset for the Big Data Economy Part 1.2
By Emily Garcia, as published by Real Left on 27 January 2026
Table of Contents
The ‘Five Year Forward View’ released in 2014
In 2014, Simon Stevens left his position as head of the global division of American health insurance giant UnitedHealth for the appointment of Chief Executive of National Health Service (“NHS”) England, a role he continued to hold until he was succeeded by Amanda Pritchard in August 2021.
His ‘Five Year Forward View’, [1] released in October 2014, faithfully adheres to both the diagnosis of the healthcare crisis and the proscribed solutions laid out by the World Economic Forum (“WEF”) Sustainable Health Systems project in which Stevens was heavily involved (see Part 1.1).
As part of the “new models of care,” Stevens oversaw the embedding of UnitedHealth’s UK subsidiary Optum into the NHS in 2015 by introducing Optum software, algorithms, personnel and business practices, and training of local council leaders. [2] He also brought in health insurance company Centene, [3] owner of Operose Health (until 2023), which is the largest general practitioner (“GP”) surgery operator in the NHS, and orchestrated Virginia Mason Hospital’s partnership with five Foundation Trusts. [4]
Simultaneously, “vanguards” in 50 areas were given the task of developing and testing these new care models. [5] The following year the NHS and local councils formed Sustainability and Transformation Partnerships (“STPs”), originally called Sustainability and Transformation Plans, covering all of England, for the delivery of the NHS Five Year Forward View [6] (“5YFV”). The STPs were rolled out to enable the wide-scale introduction of Accountable Care Organisations (“ACOs”) and Accountable Care Systems (“ACSs”) from 2018. [7] These were first trialled in the NHS at three beacon sites from 2003, as mentioned in Part 1.1.
Michael MacDonnell, another participant in both the WEF and Imperial College’s Institute for Global Health Innovation initiatives (as Senior Fellow at the Centre for Institute of Global Health Innovation), acted as head of policy for the Sustainability and Transformation Plans framework as a whole. Ron Webster and Amanda Doyle, who were also WEF workshop participants, were tasked with leading individual STPs in West Yorkshire and in Lancashire and South Cumbria, respectively. [8]
The initial introduction of ACOs, which were characterised by Keep Our NHS Public as “autonomous business units” unaccountable tolocal populations or Parliament, and “motivated by accountancy, and managed by financiers,” [9] proved highly controversial. Two separate legal actions were launched to challenge them in 2017. [10]
One of the groups that lodged a judicial review, “999 Call for the NHS,”argued that the ACO contracts’ shift to a single, annual budget for a population, rather than a payment by services used model, breached sections 115 and 116 of the Health and Care Act 2012. [11]
Although both challenges were ultimately unsuccessful, as a consequence the government was forced to delay ACO implementation until a public consultation had been carried out. In addition, following the bad publicity around ACOs, a name change to Integrated Care Boards or Systems was instituted. This paralleled a similar scenario in the US. ACOs were called Health Maintenance Organisations (“HMOs”) until 2013 when Kaiser changed the name in response to HMOs falling into disrepute, due to lawsuits which alleged that they were denying patients care and not enrolling expensive patients. [12]
The contention over the legality of erasing the NHS’s founding principle of “equal care for equal need,” through allowing ACOs or Integrated Care Systems’ full control over budget spending, was rendered moot through changes introduced in the 2022 Health and Social Care Act (covered in Part 1.3).
Returning to key features of the “new models of care,” one of these was the introduction of multi-speciality community providers, i.e., primary care super-hubs, which would aim to “shift the majority of outpatient consultations and ambulatory care out of hospital settings,” [13] and reduce specialist care facilities. [14] Further cost savings were sought through expanding the roles of less qualified staff to facilitate a cheaper workforce. [15]
As a result of new funding models introduced in the 5YFV, including the phase out of the Minimum Practice Income Guarantee from 2014, which made smaller practices financially unviable in many cases, a large-scale progressive closure of GP practices occurred. [16] A rare event pre-2013, the rate of GP surgery closures has since risen to between 2-8 a week, with a resulting 1398 practices in England alone lost by May 2023. [17]
Unsurprisingly, the transformation of digital care was another important focus. This was to be achieved through introducing interoperable electronic health records, expanding the set of NHS-accredited health apps to help patients manage their own health and care and making online GP appointments and repeat prescription requests routinely available. [18]
The 5FYV also set out the intention for the NHS to become one of the best places in the world to “test innovations that require staff, technology and funding all to align in a health system, with universal coverage serving a large and diverse population.” [19]
Amongst the “mechanisms” used to achieve such a vision were plans for “health and care new towns,” which would integrate “not only health and social care, but also other public services such as welfare, education and affordable housing.” [20] The NHS Test Bed and Trials programme is also mentioned and described as, “real world sites for ‘combinatorial’ innovations that integrate new technologies, bioinformatics, new staffing models and payment-for-outcomes.” [21]
The NHS Healthy New Towns Project Begins in 2015
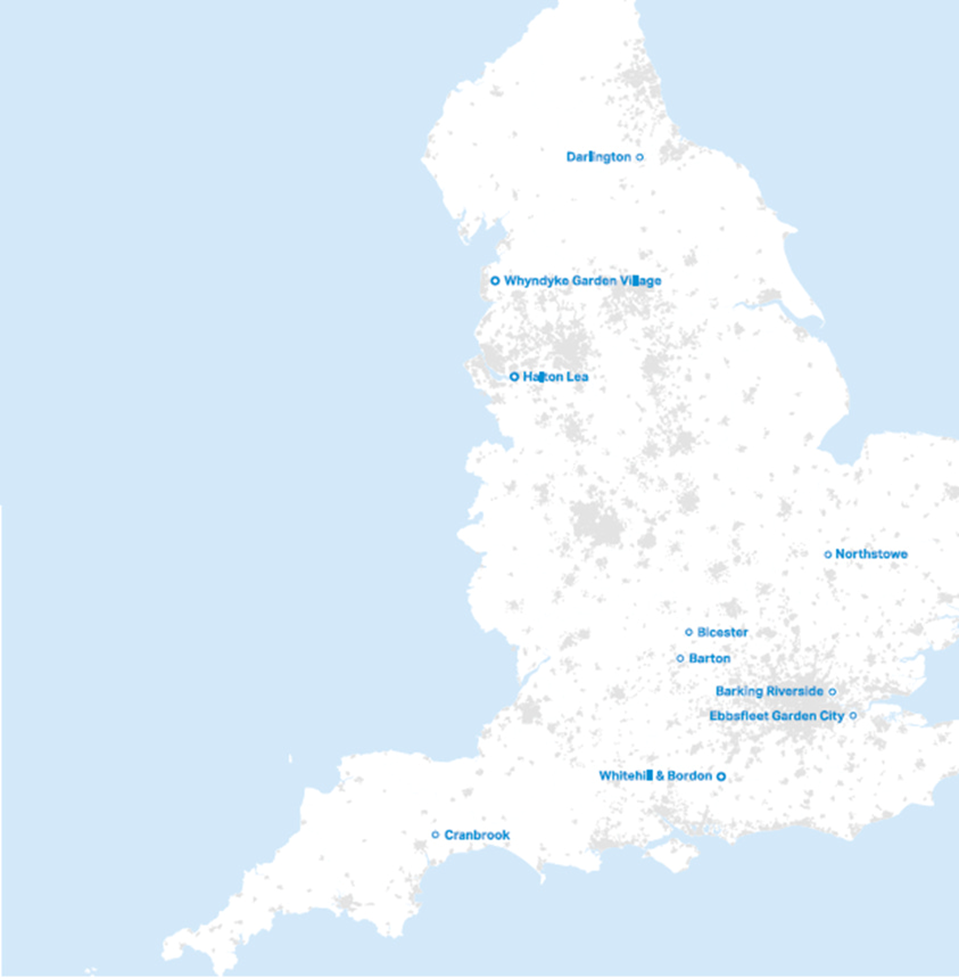
The NHS has been involved in the roll-out of Internet of Things (“IoT”) connected homes since 2015 through their Healthy New Towns project; followed by the test beds and trials programmes in 2016 and 2018, [22] as well as more recent initiatives that will be covered in Part 2.1 of this series.
Ten sites for Healthy New Towns were selected from across England and Scotland to showcase “new models of technology-enabled primary care,” [23] and “digitally enabled local health services that share physical infrastructure and staff with schools and community groups.” Construction of the exemplar healthy communities began in 2015-2016 and is ongoing.

The “key lessons” from the Healthy New Towns programme were distilled into four publications overseen by a team drawn from the NHS, Public Health England, the Town and Country Planning Association, The King’s Fund, The Young Foundation and PA Consulting. [24]

‘Putting health into place: principles’ 9-10 states:
To support the growth of the new and integrated approaches to health and wellbeing described in Principle 9, new developments need buildings that help to break down the traditional boundaries between different services. One of the important ways this can be done is through co-locating key services into health and wellbeing centres or community hubs, bringing together GP practices, other health care services, and a range of leisure, education, wellbeing and community activities in one place (see Principle 7). [25]
The blurring of spatial boundaries between healthcare and other public facilities in the built environment, and of caregiver boundaries between professional medical staff, VCSE service deliverers and “peer supporter/signposters” [26] are stated goals of an “assets based” approach, [27] explored in more detail in ‘The Wigan Deal’ section below [see next article published by The Exposé].

This approach has been carried over into the practice of boundaryless pooling of resident data. In the Darlington project, NHS England boasts of establishing effective data sharing between available health, social care, local authority and voluntary organisation sources, alongside building smart houses in neighbourhoods with “built in monitoring and information access.” [28]
Similarly, Whyndyke Garden Village has developed a digital masterplan with a “platform for affordable smart homes and digital community infrastructure.” [29] A “smart home” is explicitly highlighted in the report ‘Putting health into place principles 4-8. Design, deliver and manage’ as one of the four criteria which can be used to create housing that “supports health and wellbeing.” [30]
Behavioural nudge strategies (as mentioned on p. 35 of the Five year forward view) to encourage the adoption of “healthier behaviours” by residents are also central to the Healthy New Towns mission. New arrivals to Northstowe receive an information pack with financial incentives to encourage “active and sustainable travel choices,” including subsidised bus tickets and money-off vouchers for cycle-training “taster” sessions and kit, as well as face-to-face advice from the “travel plan co-ordinator.” [31] Citiesmode was selected as “competition winner” by NHS England and the local clinical commissioning group, to design the “Halton Connected” programme, which includes the offer of an internet app for local residents that rewards walking with discounts at local shops. [32]
The creator of Ebbsfleet Garden City, Ebbsfleet Development Corporation, funded a local version of the BetterPoints scheme until at least 2022-23. This smartphone app encouraged local residents to record their walking, wheeling, running and cycling activities in exchange for points, which were redeemable as vouchers at selected outlets, charity donations or entries in prize draws. [33]
BetterPoints has been delivering incentivised smartphone app-based behaviour change programmes since 2010, primarily in collaboration with local councils. [34]

These programmes combine active travel goals with public health objectives such as reduction of smoking or obesity in the target population.
Public Health Principal at Buckinghamshire Council, Sally Hone, is quoted in a BetterPoints return on investment case study endorsing the scheme: “The app being led by behaviour change and the COM-B model means it complements the wider work being done in Public Health.” [35]
The app incorporates gamification and geofencing features that enable clients to set specific zones for activities and rewards for the users of their tailored app.

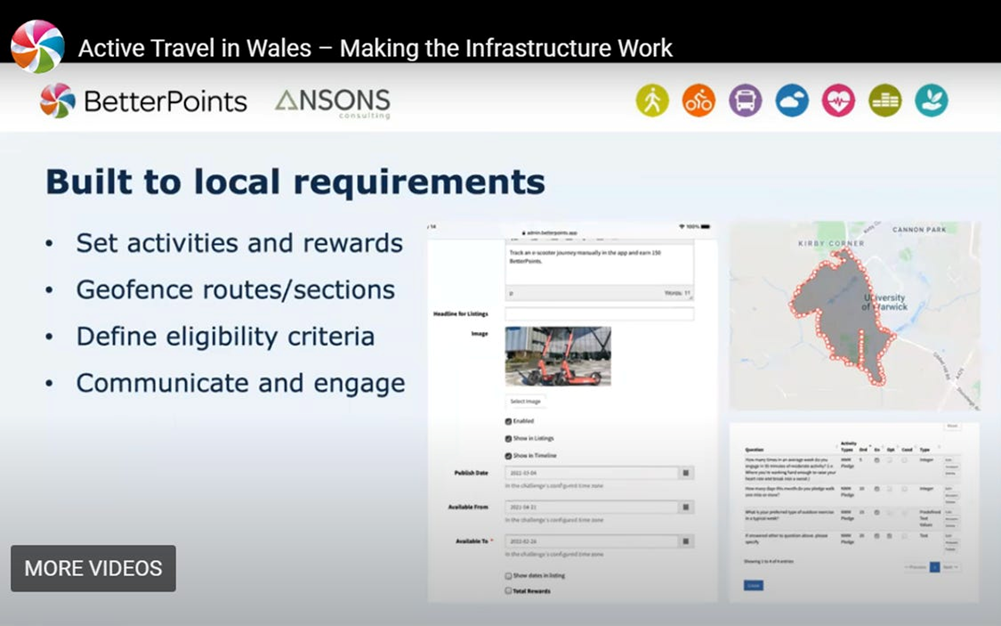
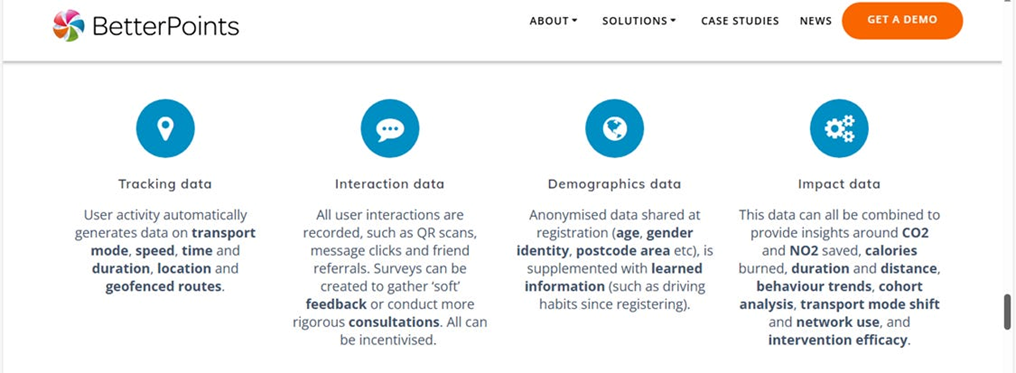
BetterPoints’ conscious positioning as players in the emerging impact economy is evidenced by their having sought and achieved the B-corp certification [36] for “positive social impact.” Additionally, they state on their website that BetterPoints programmes are “designed to align with UN Sustainable Development Goals and to help achieve them.” To do so, clients are provided a dashboard that allows them to “track and measure their impact” on key indicators, including “carbon and nitrogen savings,” achieved by altering the travel or other behaviours of the target cohort of app users. These dashboards, they explain, enable clients to “configure graphs, charts and heatmaps, for example for ESG reporting, strategy analysis, infrastructure planning, and healthcare monitoring.” (My emphasis.) [37]
[To be continued.]
References
- [1] NHS England. Five Year Forward View. October 2014. [Online]: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
- [2] Cave, T. ‘Why are GPs being Told to Hand Billions-Worth of NHS Decisions to Private Health Firms and Their Lobbyists?’ OpenDemocracy. 3 May 2015. [Online]: https://www.opendemocracy.net/en/ournhs/why-are-gps-being-told-to-hand-decisions-to-private-health-firms-and-their-lobbyists/ (https://archive.is/k33Tg).
- [3] Public Matters. Health and Care Bill 2021: the NHS, the law, and democracy. YouTube; 26 July 2021. [Online video]:
- (Timestamp, from 05:50.)
- [4] Burgess, N., Currie, G., Crump, B., Dawson, A., (2022) Leading change across a healthcare system: How to build improvement capability and foster a culture of continuous improvement. Report of the evaluation of the NHS-VMI partnership. Warwick Business School; Spring 2022. [Online]: https://warwick.ac.uk/fac/soc/wbs/research/vmi-nhs/reports/report_-_leading_change_across_a_healthcare_system_22.09.2022.pdf
- [5] NHS England. New Care Models: Vanguards – developing a blueprint for the future of NHS and care services. September 2016 [Online]: https://www.england.nhs.uk/wp-content/uploads/2015/11/new_care_models.pdf
- [6] Pickett, L. Sustainability and transformation plans and partnerships: Briefing paper CBP-8093. House of Commons Library; 29 September 2017. [Online]: https://researchbriefings.files.parliament.uk/documents/CBP-8093/CBP-8093.pdf p. 3
- [7] NHS Providers. STPs And Accountable Care, background briefing. 15 January 2018. [Online]: https://nhs-providers.uksouth01.umbraco.io/media/zq4fxsrv/stps-and-accountable-care-background-briefing-january-2018.pdf p. 7
- [8] Player, S. ‘The Truth about Sustainability and Transformation Plans: How Simon Stevens Imposed a Reorganisation Designed for Transnational Capitalism on England’s NHS.’ Socialist Health Association; 31 October 2021. [Online]: https://sochealth.co.uk/2017/05/25/truth-stps-simon-stevens-imposed-reorganisation-designed-transnational-capitalism-englands-nhs-stewart-player/ (https://archive.is/Btfg3)
- [9] O’Sullivan, T. ‘Judicial Review 23/24 May Challenging Legality of Introduction of ACOs.’ Keep Our NHS Public. 21 May 2018. [Online]: https://keepournhspublic.com/judicial-review-23-24-may-challenging-legality-of-introduction-of-acos/
- [10] Bate, A. Accountable Care Organisations. Briefing paper CBP-8190; House of Commons Library. 6 July 2018. [Online]: https://commonslibrary.parliament.uk/research-briefings/cbp-8190/ p. 15
- [11] Ibid.
- [12] Harrington, H., Ormerod, J. ‘Accountable Care Organisations: Their potential impact on delivery of health & social care to patients in England’s NHS.’ Public Matters. January 2018. [Online]: https://publicmatters.org.uk/wp-content/uploads/2018/01/Accountable-Care-Organisations-briefing-final.pdf p. 10
- [13] NHS. Five Year Forward View. NHS England. October 2014. [Online]: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf p. 19
- [14] Ibid., p. 23
- [15] Ibid., p. 19
- [16] Carter, R., Kaffash, J. ‘Why GP practices close for good.’ Pulse Today. 5 September 2022. [Online]: https://www.pulsetoday.co.uk/analysis/lost-practices/why-gp-practices-close-for-good/ (https://archive.is/awykS)
- [17] Checkland, K., Gibson, J., Hutchinson, J., Kontopantelis, E., Sutton, M. ‘Consequences of the Closure of General Practices: a Retrospective Cross-Sectional Study.’ British Journal of General Practice. 16 May 2023. [Online]: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10227999/ (https://archive.is/4QgWk)
- [18] NHS. Five Year Forward View. NHS England. October 2014. [Online]: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf p. 32
- [19] Ibid., p. 34
- [20] Ibid., p. 35
- [21] Ibid., p. 34
- [22] Galea, A., Hough, E., Khan, I. Test Beds the story so far. NHS England: London; 2017. [Online]: https://www.england.nhs.uk/wp-content/uploads/2017/09/test-beds-the-story-so-far.pdf
- [23] NHS England. ‘NHS Chief announces plan to support ten healthy new towns.’ 1 March 2016. [Online]: https://www.england.nhs.uk/2016/03/hlthy-new-towns/ (https://archive.is/TOtj5)
- [24] NHS England. ‘Healthy New Towns.’ [Online]: https://www.england.nhs.uk/ourwork/innovation/healthy-new-towns/ (https://archive.is/8zCdF)
- [25] NHS England. Putting health into place principles 9-10: develop and provide healthcare services. London; September 2019. [Online]: https://www.england.nhs.uk/wp-content/uploads/2019/09/phip-3-develop-provide-healthcare.pdf p. 22
- [26] Ibid., p. 14
- [27] Ibid., p. 14
- [28] NHS England. ‘Healthy New Towns: Demonstrator Sites: Darlington.’[Online]: https://www.england.nhs.uk/ourwork/innovation/healthy-new-towns/demonstrator-sites/darlington/ (https://archive.is/6sxIb)
- [29] NHS England. ‘Healthy New Towns: Demonstrator Sites: Whyndyke.’[Online]: https://www.england.nhs.uk/ourwork/innovation/healthy-new-towns/demonstrator-sites/whyndyke/ (https://archive.is/hkIeX)
- [30] NHS England. Putting health into place principles 4-8: design, deliver and manage. London; September 2019. [Online]: https://www.england.nhs.uk/wp-content/uploads/2019/09/phip-2-design-deliver-manage.pdf p. 38
- [31] Ibid., p. 22
- [32] Hefma (Health estates and facilities management association). ‘NHS competition challenges ideas to design for life.’ [Online]: https://www.hefma.co.uk/news/nhs-competition-challenges-ideas-to-design-for-life (https://archive.is/k0fWH)
- [33] BetterPoints. Motivating healthy activity in Ebbsfleet Garden City. 31 October 2023. [Online]: https://www.betterpoints.ltd/download/motivating-healthy-activity-in-ebbsfleet-garden-city/ (https://archive.is/UJHVx)
- [34] BetterPoints.‘Active Travel in Wales – Engagement and Communication is Crucial, Webinar Attendees Told.’ 29 July 2021. [Online]: https://www.betterpoints.ltd/blog/active-travel-in-wales-engagement-and-communication-is-crucial-webinar-attendees-told/ (https://archive.is/7Nzgn)
- [35] BetterPoints. Buckinghamshire behaviour change programme paid for itself four times over. 29 May 2024. [Online]; Available to download at: https://www.betterpoints.ltd/download/buckinghamshire-behaviour-change-programme-paid-for-itself-four-times-over/ p. 2 of report
- [36] B Corporation UK. ‘B Corp Certification.’ [Online]: https://bcorporation.uk/b-corp-certification/ (https://archive.is/GQgHd)
- [37] BetterPoints. ‘About us.’ [Online]: https://www.betterpoints.ltd/about-us/ (https://archive.is/ARgej)
Featured image taken from ‘NHS75 – History of the NHS’, NHS North East London, 4 July 2023
The Expose Urgently Needs Your Help…
Can you please help to keep the lights on with The Expose’s honest, reliable, powerful and truthful journalism?
Your Government & Big Tech organisations
try to silence & shut down The Expose.
So we need your help to ensure
we can continue to bring you the
facts the mainstream refuses to.
The government does not fund us
to publish lies and propaganda on their
behalf like the Mainstream Media.
Instead, we rely solely on your support. So
please support us in our efforts to bring
you honest, reliable, investigative journalism
today. It’s secure, quick and easy.
Please choose your preferred method below to show your support.
Categories: Breaking News, UK News

https://www.youtube-nocookie.com/embed/NIrg9iB4z7Y trump and family lol
https://www.youtube-nocookie.com/embed/C_qvTKgJbt4 trump and wife lol heating up
🙏🙏
What the Holy Bible says of this horrific decade just ahead of us.. Here’s a site expounding current global events in the light of bible prophecy.. To understand more, pls visit 👇 https://bibleprophecyinaction.blogspot.com/
https://www.youtube-nocookie.com/embed/5QeMvbsiQI0 the third obelisk ( Vatican )
https://www.youtube-nocookie.com/embed/jYZksdzVxic this is good
Thoroughly nauseating. Carbon and Nitrogen? Do these morons think we are running around leaving chunks of coal or diamonds everywhere? That’s Carbon. Of course Carbon dioxide is the gas of life on this plant planet, demonised by that cretin Obama.. and Nitrogen? 78% of the far king atmosphere is Nitrogen! And its a gas of life too. What next? Demonising Dihydrogen monoxide? That’s water by the way. The world is a sorry mess. Time for a reset AWAY from the UNs ideas. Warmongers and eugenics loonies.